A 32-year-old female patient initially dismissed mild pelvic discomfort and light spotting as irregularities in her menstrual cycle. She assumed they were related to ovulation. However, when the ovulation test came back negative, she tried a home pregnancy test, which to her surprise, was positive.
Unfortunately, a few hours later, she had to be rushed to the hospital because of severe pain on one side of her abdomen accompanied by vaginal bleeding. Ultrasound findings revealed no gestational sac in her uterus but confirmed implantation in one of her fallopian tubes, which had ruptured and was causing internal bleeding. An emergency surgery was performed to stop the bleeding and remove the pregnancy along with the ruptured Fallopian tube.

The current example illustrates a classic case of ectopic pregnancy. This condition, despite its rarity, presents significant challenges and dangers to women’s health. Unfortunately, there’s a pervasive lack of awareness and understanding about it.
In this blog, we’ll delve into various aspects of ectopic pregnancies, addressing important questions and concerns related to this condition. We aim to highlight the crucial importance of early detection and appropriate medical intervention in effectively managing this condition.
What is Ectopic Pregnancy?
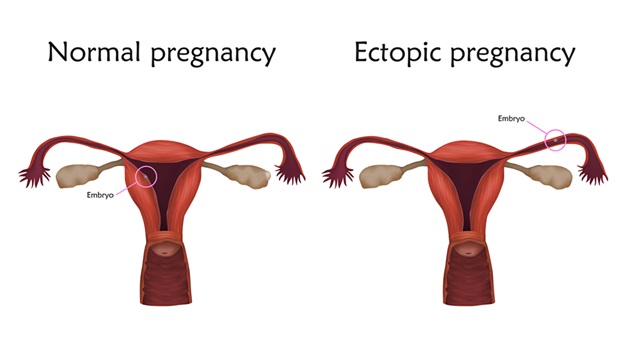
An ectopic pregnancy occurs when a fertilized egg implants and grows outside the uterus. The term “ectopic” is derived from the Ancient Greek roots ἐκτόπος, meaning “out of place.” Also known as extrauterine pregnancy, over 95% of these cases involve implantation in the fallopian tube.
Worldwide, approximately 1-2% of naturally conceived pregnancies result in ectopic implantation. Over the past 30 years, global morbidity and mortality associated with ectopic pregnancy (EP) have decreased. However, economically disadvantaged regions continue to see increasing rates.
In the United States, EPs constitute 1-2% of all pregnancies; in Africa, rates range from 1.1% to 4.6%; and in the United Kingdom, the incidence was 11.1 per 1,000 pregnancies. In India, incidence ranges from 0.91% to 2.3%, primarily among women aged 20-30 years from the lower middle class. Public health policies should address disparities, provide protection for vulnerable women, and prioritize early EP diagnosis and treatment.
Where does an ectopic pregnancy occur?
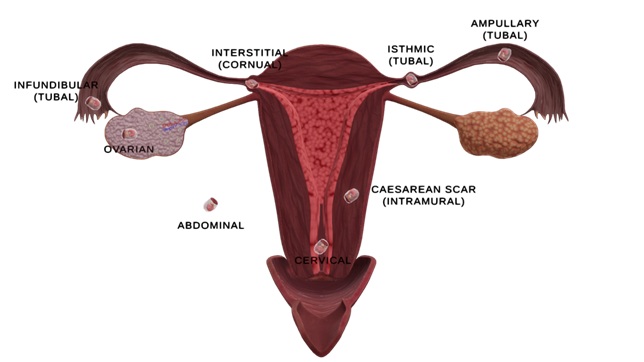
Ectopic pregnancies can manifest in various locations within the female body. Depending on the site of implantation, the most common type is tubal ectopic pregnancy, where the egg implants in the fallopian tube. Based on the location in the fallopian tube, tubal pregnancy can be an infundibular/fimbrial, ampullary or isthmic type of ectopic pregnancy. The ampulla of the fallopian tube is the predominant site of implantation for tubal pregnancies (80%), followed by the isthmus (12%), fimbria (5%), cornua (2%), and other locations (1%).
Cesarean scar ectopic pregnancy occurs when the gestational sac implants into the anterior uterine wall where a previous cesarean scar is present.
Cervical ectopic pregnancy occurs when the gestational sac implants in the mucosa of the endocervical canal, presenting both high complications and high treatment success rates.
Ovarian ectopic pregnancy involves implantation in the ovaries, often associated with intrauterine devices.
Abdominal ectopic pregnancies are exceedingly rare and occur when the gestational sac implants in the peritoneal cavity of the abdomen, where most abdominal organs reside.
Cornual ectopic pregnancies occur when implantation happens in the uterine horns. These structures, also known as the cornua of the uterus, are located in the upper uterus, where the fallopian tubes or oviducts extend to connect with the ovaries.
What are the signs and symptoms of an Ectopic Pregnancy?
In the initial stages, an ectopic pregnancy may not manifest noticeable symptoms or may present symptoms akin to those of a normal pregnancy, such as absence of regular menstruation, breast tenderness, nausea, vomiting, and fatigue. However, as the pregnancy progresses, more specific symptoms may emerge. These symptoms include:
- Pelvic or Lower Abdominal Pain: Ranging from mild to severe, this pain may be constant or intermittent, typically initiating on one or either side of the abdomen and radiating to the shoulder or neck.
- Vaginal Bleeding or Spotting: Light or heavy bleeding may occur, often differing from a regular period by starting and stopping and appearing watery and dark brown in color. Some may mistake this bleeding for a typical period, unaware of the pregnancy. While common in pregnancy, vaginal bleeding warrants medical advice.

- Shoulder tip pain: Shoulder pain during pregnancy can arise for numerous reasons and is frequently normal. However, if you notice pain in your shoulder tips early in the first trimester, it might be due to blood leaking from your fallopian tube into your abdomen. This leakage can irritate the phrenic nerves that innervate the diaphragm, which the brain interprets as pain in the shoulder tip region.
- Discomfort When Using the Toilet: Pain or pressure during bowel movements, urination pain, or diarrhea may occur. While some changes are normal during pregnancy, seeking medical advice is prudent.
Emergency Symptoms
Ectopic pregnancies are the primary cause of maternal mortality in the first trimester, responsible for 5%-10% of all pregnancy-related deaths. If an ectopic pregnancy advances undetected, there is a considerable chance that the site of implantation will rupture. Such a scenario is a medical emergency as rupture can cause massive internal bleeding resulting in shock, sharp abdominal pain, nausea, dizziness, extreme lightheadedness, and fainting.
When do the symptoms of ectopic pregnancy start?
Notably, not all women exhibit symptoms, and some may remain asymptomatic, particularly in the early stages. However, the first warning signs can usually be felt, between the 4th and 12th weeks of pregnancy. In some instances, the presenting symptoms of acute appendicitis and ectopic pregnancy, particularly a right-sided ectopic pregnancy, can overlap.
Acute appendicitis typically begins with poorly localized periumbilical pain that shifts to the right lower quadrant. In cases of ectopic pregnancy, the pain can mimic these classic symptoms. Therefore, it is crucial for surgeons to conduct urine pregnancy tests (UPT) for females of reproductive age to ensure an accurate diagnosis.
How is an ectopic pregnancy detected?
Early detection of ectopic pregnancy is crucial for timely intervention. As ectopic pregnancy mimics the normal constellation of pregnancy symptoms, diagnosing it can be challenging, especially in its early stages.
A physician typically conducts a pregnancy test to confirm conception. They also perform a pelvic exam to identify areas of pain, tenderness, or abnormalities in the fallopian tubes or ovaries.
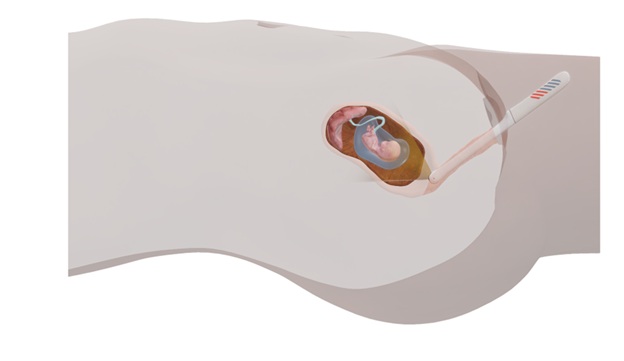
The diagnosis of an ectopic pregnancy is considered when a blood test reveals elevated levels of β-HCG; and an ultrasound confirms the absence of a viable intrauterine pregnancy. Transvaginal ultrasound is particularly effective in confirming the diagnosis of ectopic pregnancy. It helps to identify the location of the extra-uterine gestational sac.
In some instances, even transvaginal ultrasound fails to identify the location of a pregnancy, leading to the diagnosis of ‘pregnancy of unknown location’ (PUL). At present, laparoscopy is typically performed in such instances, especially when symptoms or signs of hemoperitoneum or blood in the peritoneal cavity are detected.
How is ectopic pregnancy different from a normal pregnancy?

In a typical pregnancy, a single sperm fertilizes an egg within the ampulla of the fallopian tube. The resulting fertilized egg then travels through the fallopian tube, where it divides to form an embryo. Eventually, the embryo reaches the uterus and implants itself into the endometrium, or the uterine lining.
In approximately one in every 50 pregnancies, implantation takes place outside the uterus. A woman experiencing an ectopic pregnancy may notice vaginal bleeding, persistent abdominal or pelvic pain, and shoulder tip pain.
The diagnostic approach is also not the same. In a normal pregnancy, a positive pregnancy test is usually followed by an abdominal ultrasound to confirm the intrauterine pregnancy. Conversely, in an ectopic pregnancy, although the initial pregnancy test may be positive, abdominal ultrasound will not reveal a viable intrauterine pregnancy.
Understanding and noticing these distinctions are critical for the early detection of ectopic pregnancy. Seek immediate medical attention, if you are experiencing any of the signs above symptoms and you are pregnant or planning to get pregnant.
Will ectopic pregnancy show β-HCG levels?
In the early stages of a typical pregnancy, the β-HCG (human chorionic gonadotropin) hormone, produced by the developing placenta, doubles every 48-72 hours until it reaches 10,000-20,000 mIU/mL. This steady rise in β-HCG levels is a marker of healthy intrauterine pregnancy.
Similar to normal pregnancies, even in ectopic pregnancies, the level of β-HCG can be observed. However, the β-HCG levels typically exhibit slower increases and tend to remain at lower levels than those of normal pregnancies./p>
It’s important to note that while β-HCG levels can provide valuable diagnostic information, it is not enough for diagnosing ectopic pregnancy. Instead, healthcare providers rely on a combination of clinical symptoms, ultrasound findings, and serial β-HCG measurements before making a definitive diagnosis.
Can ectopic pregnancy come to term?
Unlike normal pregnancies, ectopic pregnancies can’t be carried to full term and neither can be transplanted into the womb. In-fact, if not immediately taken care of, they can lead to hemorrhage, infections and even death.
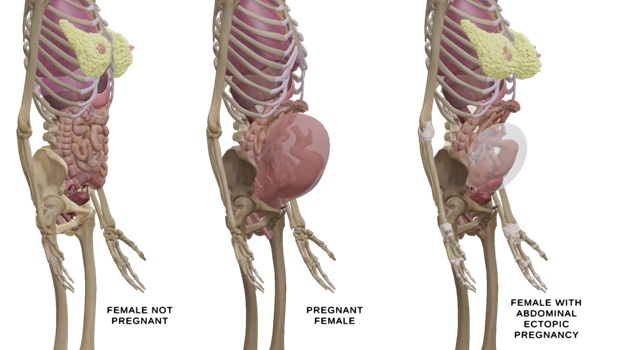
In some very rare cases, studies have described live births resulting from abdominal ectopic pregnancies. Nonetheless, survival of a fetus in an abdominal pregnancy is exceedingly uncommon. Neonates who do survive often experience a high incidence of fetal deformities and perinatal death.
A case report published in The New England Journal of Medicine, described a gravida presented with a 10-day history of abdominal pain, prompting medical evaluation. Upon physical examination, clinicians suspected an abdominal pregnancy. The patient had a history of two full-term deliveries and one miscarriage.
Ultrasonography revealed a thickened endometrium, but no intrauterine gestational sac. Further imaging with MRI confirmed a 23-week abdominal pregnancy, with the fetus attached to a placenta implanted on the abdominal lining above the sacral promontory.
Given that ectopic pregnancies cannot be sustained to full term that is 37-41 weeks, at 29 weeks gestation, a laparotomy was performed, resulting in the delivery of the infant, who was subsequently admitted to the neonatal intensive care unit. The initial procedure included partial placental removal, with the remainder excised in a follow-up surgery. The patient was discharged 25 days postpartum, and approximately one month later, she was able to bring her baby home.
What are the options for treating ectopic pregnancy?
The management of ectopic pregnancy depends on several factors, including the location and size of the ectopic pregnancy, the woman’s overall health, and her desire for future fertility. Here are the common treatment options:
- Expectant Management: In instances, when an ectopic pregnancy is identified in its early stages and hormone levels are still relatively low, healthcare providers may opt for close monitoring, allowing the pregnancy to be naturally absorbed by the body over time.
- Medication with Methotrexate: Methotrexate is the primary medication employed for terminating an ectopic pregnancy. It halts embryonic growth, enabling the body to absorb residual tissue. This treatment is appropriate for early-detected ectopic pregnancies with low hormone levels and no rupture.
- Surgical Intervention (Laparoscopy): Laparoscopic surgery is performed by making a small incision to access the fallopian tube and remove the ectopic pregnancy. The primary goal of this procedure is to preserve the fallopian tube whenever feasible. It is usually recommended when the ectopic pregnancy has ruptured or when medication is deemed unsuitable or ineffective.
- Surgical Removal (Laparotomy): In rare and severe cases where the ectopic pregnancy has resulted in substantial damage, healthcare providers may opt to perform a more invasive laparotomy. In some instances, part or all of the affected fallopian tube may also need to be removed.
Why does an ectopic pregnancy happen?
An ectopic pregnancy happens due to various reasons. The risk factors that can disrupt the normal course of uterine implantation include:

- Abnormalities in Fallopian Tubes: Structural abnormalities in the fallopian tubes, such as congenital defects or abnormal growths, can obstruct the egg’s movement and increase the likelihood of the egg implanting and growing in the tube itself. This can result from conditions like pelvic inflammatory disease (PID), previous pelvic surgeries (such as tubal ligation reversal or appendectomy), or scarring from prior ectopic pregnancies.
- Hormonal Factors: Imbalances in the hormonal factors that affect the movement of the fertilized egg through the fallopian tube and into the uterus can contribute to ectopic pregnancies.
- Endometriosis: Women diagnosed with endometriosis, a condition characterized by the growth of uterine lining tissue (endometrium) outside the uterus, may develop scar tissue or adhesions that can impair the function of the fallopian tubes. This condition heightens the risk of an ectopic pregnancy.
- Previous Surgeries or Infections: Surgeries on the fallopian tubes or pelvic area, as well as infections that affect the reproductive organs (such as pelvic inflammatory disease), can lead to scarring or damage that predisposes to ectopic pregnancies.
- Fertility Treatments: Women undergoing fertility treatments, especially procedures like in vitro fertilization (IVF), have a slightly higher risk of ectopic pregnancy. This is due to factors related to embryo transfer and the altered environment of the reproductive system during treatment.
- Other Factors: Certain lifestyle choices like smoking, advancing maternal age (especially over 35), and a history of ectopic pregnancy itself can also increase the risk.
In Conclusion
Ectopic pregnancy is a serious medical condition that requires appropriate management to prevent complications and preserve fertility. By educating ourselves and others about ectopic pregnancy, we can raise awareness, promote early detection and in turn foster a supportive and understanding environment for those impacted by this challenging condition.
Writer – Dr. Debashree Das
Medical Content Writer